
Amulya Cherukumudi
Department of General Surgery, KS Hegde Medical Academy, Deralakatte, Mangaluru-575018, Karnataka, India.
*Corresponding authors: Amulya Cherukumudi, Department of General Surgery, KS Hegde Medical Academy, Deralakatte, Mangaluru-575018, Karnataka, India.
Received Date: July 24, 2023
Accepted Date: August 18, 2023
Published Date: August 31, 2023
Citation: Amulya Cherukumudi (2023). “Step-Wise Ligation of Hilum Vs Mass Ligation During Lobectomy of The Lung- Is it Time for A Change?”. Clinical Research and Clinical Case Reports, 4(1); DOI: http;//doi.org/08.2023/1.1058.
Copyright: © 2023 Amulya Cherukumudi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Lobectomy of the lung has been done over from the early 1700s for various causes, from trauma to tumour, and has had varying percentage of success. The technique has since been improved upon, and we have landed in the era of video-assisted and robotic lobectomy of the lung. [1]
Introduction:
Lobectomy of the lung has been done over from the early 1700s for various causes, from trauma to tumour, and has had varying percentage of success. The technique has since been improved upon, and we have landed in the era of video-assisted and robotic lobectomy of the lung. [1]
From rib resections to minimal access surgery, lobectomy has come leaps and bounds. However, it is not without complications post-operatively. [2]
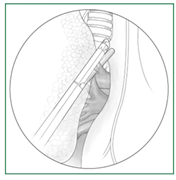
The standard technique for lobectomy followed now is using the superior hilar approach and the bronchus first technique, where the pulmonary artery (PA) vessels are first divided. The conduct of RAL necessitates some degree of adaptation due to the fact that structures may be recognized and split in a systematic orderly manner or in the sequence that the patient’s particular anatomy permits. The latter is usually preferred in order to manipulate and flip the lung as little as possible because the lymphadenectomy dissection started in the back of the lung. [3,4]

However, there are certain scenarios where adhesions or extensive lymphadenopathy at the hilum have distorted the vessels. Also, in case of tumors and fistulae, the bronchus and vessels may be in close proximity. Hence, it may be necessary to perform a mass ligation of the hilar structures.
The separate dissection of the lobe's vein, artery, and airway forms the basis of lobectomy. The anterior approach, often known as the anterior mediastinum, is currently the most common. In a single direction, from anterior to posterior, the dissection sequence is performed.[5-7] The recent surgical practice of dividing the pulmonary fissures by direct stapling over the visceral pleura is known as the "fissure-less technique."[8] The fissure-last approach exposes artery structures by opening the fissure toward the end of surgery.[9] Surgery is known as the fissure-first procedure (tunnel technique) if the fissure is opened first. However, the fissure-less technique has been the suggested method due to the low risk of postoperative air leaks. The fissure-first technique merits consideration when the hilum dissection is complicated and the vascular and bronchial structures plane dissections are difficult to identify[10-11]
To our knowledge, there is limited data to compare the outcomes of step-wise ligation with mass ligation at the hilum for lobectomy.
Methods and Materials:
This was a retrospective study performed in a tertiary care hospital affiliated with a medical college. A total of 40 participants were included in the study, between ages 18-70, undergoing lobectomy under GA and for benign causes.
Those patients with malignancy of the lung, diffuse involvement of the lung requiring extension to pneumonectomy, bilateral lung lesions, and previous surgery to the chest were excluded from the study.
Group A- step-wise ligation of the vessels ( n=20)
Group B- mass ligation of the hilum ( n=20)

Demographic details, clinical history, and details of the surgery were collected and recorded in a semi-structured pro forma. The data was then entered in an MS Excel spreadsheet, and the data was analyzed using SPSS V21. categorical variables were represented as Frequency and Proportion, while continuous variables were represented as mean and SD. T-test and Chi-square test were used where appropriate. A p-value less than 0.05 was considered statistically significant.
Primary outcomes were bleeding and air leak intra-operatively, operative time.
Secondary outcomes were stump blowout, need for re-exploration, ligature slippage, bronchopleural fistula, ICU stay, and hospital stay, death.
Any other complications were also noted and analyzed. The demographic factors, etiology and other parameters were then correlated to the procedure done.
Results:
A total of 40 participants were taken up for the study, and divided into two groups by the surgery team. Group A underwent step wise bronchus first approach to hilar ligation, while Group B underwent mass ligation.
Both the groups were age and sex matched, and the data was compared.
|
Indications for lobectomy |
Group A |
Group B |
|
Hydatid cyst |
3 |
3 |
|
Infected tubercular cavity/abscess |
6 |
5 |
|
Aspergilloma |
5 |
6 |
|
Bronchiectasis |
2 |
4 |
|
others |
4 |
2 |
Group A and B has comparable mean ages 34.61 years vs 33.58 years respectively, p value 0.973
Group A has a higher proportion of males as compared to Group B, 6 vs 4, however, the difference was not statistically significant. (P value 0.852)
Mean operative time was significantly higher in Group A than Group B ( 118.23 vs 97.48 mins; p-value 0.003).
Mean bleeding intra-operatively was significantly lower in group A than in group B ( 184.56 ml vs 236.67 ml; 0.0012)
ICD is retained in all patients with air leaks until the primary surgeon is convinced that there is spontaneous closure of the bronchopulmonary fistula. The air leak was noted in only one patient in Group A, but 3 patients in Group B, the difference was not statistically significant. All these patients required re-exploration in view of the persistent air leak.
|
Complications |
Group A |
Group B |
|
Air leak |
1 |
3 |
|
Re-exploration |
3 |
6 |
In 3 patients in Group B, there was more than 500 ml bleeding in ICD in the first hour, warranting re-exploration. We observed that there was slippage of the ligature in 1 patient, and varied anatomy in the remaining two. We, however, did not observe any massive bleeding in patients with group A. this difference was found to be statistically significant (p-value 0.0039)
The mean ventilation days was 1.56 +/- 0.76 days in group A, while it was 2.11 +/- 0.77 days in group B were not statistically different between both groups.
There was no mortality in either group of the study.
Discussion:
The preferred approach for tackling the hilar structures in a lobectomy is either bronchus first or artery first approach. However, it is observed that in certain scenarios, neither maybe feasible. Applying a mass ligature helps tackle that challenge.
The disadvantages of mass-ligation depending on the site of lobectomy is as follows:
The optimal ligature for hilar vessels when being treated in bulk was determined through an experimental investigation conducted in 1936 by Philip Shambaugh and colleagues. In order to effectively treat inflammatory lung illnesses, lobectomy and pneumonectomy must typically be performed by mass ligating the hilum rather than dissecting and ligating each individual structure. If the lung is promptly removed, the mass ligature must be tight enough to create an ischemic necrosis or to stop bleeding if the lung is left in place. By using common suture materials, a successful bulk ligation is frequently difficult to achieve. Carr came up with a solution to get around this problem by securing a cord snare in place with a metal key that is allowed to slough off with the lung. After the lung or lobe was removed, Archibald and Bethune utilised a silver wire that was twisted into place and left in place.
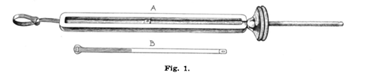
As a member of the aforementioned team, Robert Zollingher discovered that a metal band, applied using Parham's method for fixing fractures, could easily perform a mass ligation. After several attempts, a band made of annealed silver that was 0.18 inches wide and 0.020 inches thick was found to be adequate. After application, the band's distal third was grooved longitudinally to prevent lateral sliding.
The chance of slippage and bleeding, however, is much higher with mass ligation, as observed in our study. The incidence of stump blowout is significantly higher as well, as evidenced by Gaskin et al.
In the past, surgeons were advised against excessive hilar dissection and individual step-wise ligation as they observed a higher risk of infection and death, as evidenced by Lilienthal et al.
In 2019, studies were performed in dogs, where.